What is Para-Oesophageal Hernia?
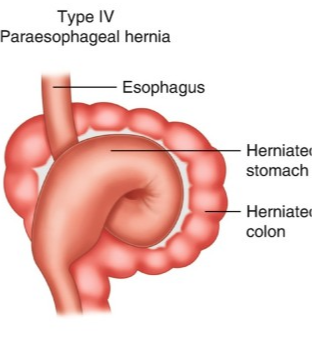
A para-oesophageal hernia, also known as a paraesophageal hernia or type II hiatal hernia, is a type of hernia that occurs when part of the stomach bulges through the hiatus (an opening) in the diaphragm and into the chest next to the oesophagus, without actually sliding into the chest cavity. This is different from a sliding hiatal hernia, which occurs when the junction between the stomach and oesophagus slides up through the hiatus and into the chest.
Para-oesophageal hernias can be asymptomatic or cause a range of symptoms including chest pain, heartburn, difficulty swallowing, and feeling full after eating small amounts. In some cases, para-oesophageal hernias can lead to more severe complications such as gastric volvulus (twisting of the stomach), strangulation, or obstruction.
Para-Oesophageal Hernia surgery Benefits
The main benefit of surgery for para-oesophageal hernia is to prevent the hernia from progressing and causing further complications. In addition, surgery can also alleviate symptoms such as chest pain, difficulty swallowing, and reflux. Some specific benefits of para-oesophageal hernia surgery include:
- Reduced risk of strangulation:
Para-oesophageal hernias can sometimes become trapped or “strangled,” which cuts off the blood supply to the herniated tissue. This can be a life-threatening complication, but surgery can help prevent it from occurring. - Improved quality of life:
Para-oesophageal hernias can cause significant discomfort and reduce quality of life, but surgery can alleviate symptoms and improve overall well-being. - Lower risk of recurrence:
Surgery can repair the hernia and reduce the risk of it recurring in the future. - Decreased need for medications:
Surgery can eliminate or reduce the need for medications used to treat symptoms of para-oesophageal hernias, such as acid reflux medications. - Prevention of complications:
Surgery can prevent other potential complications of para-oesophageal hernias, such as bleeding or ulceration of the herniated tissue.
Para-Oesophageal Hernia Procedure
The surgical procedure for para-oesophageal hernia repair typically involves the following steps:
- General anesthesia:
The patient is given general anesthesia to ensure they are unconscious and do not feel any pain during the procedure. - Laparoscopic approach:
Most para-oesophageal hernia repairs are done using a laparoscopic approach, which involves making several small incisions in the abdomen and using a laparoscope (a thin, lighted tube with a camera) and other specialized instruments to repair the hernia. - Reduction of the hernia:
The surgeon carefully pushes the herniated portion of the stomach back down into the abdominal cavity. - Repair of the hiatus:
The surgeon then repairs the defect in the diaphragm (hiatus) through which the hernia protruded, usually with stitches or mesh. - Fundoplication:
If the patient also has gastroesophageal reflux disease (GERD), the surgeon may perform a procedure called fundoplication, which involves wrapping the upper part of the stomach around the lower part of the oesophagus to create a valve that prevents stomach acid from flowing back up into the oesophagus. - Closure of incisions:
The incisions in the abdomen are closed with sutures or surgical staples, and a dressing is applied.
The duration of para-oesophageal hernia surgery depends on several factors, such as the size and complexity of the hernia, the surgeon’s experience, and the approach used (laparoscopic or open). On average, laparoscopic surgery takes about 2-4 hours, while open surgery may take longer, up to 4-6 hours.
Frequently asked questions
Paraesophageal hernias can cause symptoms such as: Difficulty swallowing (dysphagia), Feeling of fullness or discomfort in the, chest or upper abdomen after eating, Heartburn or acid reflux, Chest pain, Shortness of breath, Vomiting blood or passing dark, tarry stools (a sign of gastrointestinal bleeding), Anemia (a low red blood cell count)
Hiatal and paraesophageal hernias are usually diagnosed with an EGD or upper endoscopy, where a flexible camera is used to evaluate the esophagus and stomach. Sometimes they are incidentally found on X-rays, CT scans, or MRIs.
According to the sources, age over 50, obesity, and smoking cigarettes are all risk factors for paraesophageal hernia.
Take charge of your health today. Schedule an appointment.
BOOK A SITTING

